ClaimLogiq announces first 15-minute itemized bill review
June 17, 2021Advancement of In-House Proprietary Technology Reduces End-to-End Complex Hospital Bill Reviews Down to Mere Minutes
ClaimLogiq, a leading independently owned healthcare payment integrity company is announcing breakthrough technology that enables a complete end-to-end hospital itemized bill review in under 15 minutes. With this latest advancement, the company continues moving ever closer to facilitating near real-time payments of facility bills.
For over a decade, ClaimLogiq has been empowering analysts with its leading claim review platform, TrueCost, reducing review times of large, complex claims from days or weeks to just hours. This 15-minute audit solution is the latest demonstration of ClaimLogiq’s innovations that simplify complex payment integrity processes.
A key component in delivering a 15-minute audit is the advancement of the ClaimLogiq’s Rapid Optical Character Recognition tool, ROCR (pronounced rocker) which converts itemized bills from PDF to electronic format in minutes. The two technologies together, ROCR and TrueCost, are the ingredients that enable the 15-minute audit solution.
Todd Hill, ClaimLogiq’s CEO stated: “Our 15-minute IBill audit is another example of our commitment to staying ahead of the curve. Removing complexity and reducing turnaround time on large claim reviews is a top priority for healthcare organizations. We believe this technology will be a game-changer for many payers and will have a very positive ripple effect throughout our industry.”
According to Mr. Hill, what is especially meaningful with this announcement is that even though the benchmark is now set at 15-minutes, teams are already completing finalized reviews in far less time in certain cases. And because ClaimLogiq has not compromised its baseline framework or architecture in implementing its 15-minute audit, reviews are still completed with the same standard of quality, accuracy and consistency that TrueCost users have come to expect.
About the ClaimLogiq Pre-pay Review Process
The 15-minute lifecycle of a claim begins with ClaimLogiq’s Operational Routing and Rules Engine (CORRE), which runs claim data through an intelligent, logic-based and payer/provider-customized rules library for a pay or pend-for-review result in under 250 milliseconds. The speed of CORRE ensures no interruption to the adjudication throughput.
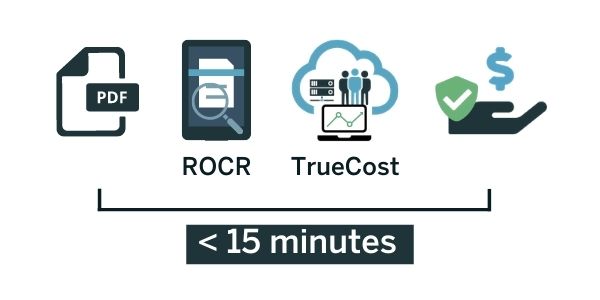
Claims pended for review are then paired with an itemized bill to be prepped for review. ROCR converts the PDF to data which is then normalized and imported into TrueCost. This process takes only a few minutes regardless of the size or file types. From here, TrueCost’s framework applies automation and payer-specific rules and edits to produce results in minutes.
ClaimLogiq’s IBill review process maintains an industry-leading standard of a less than five percent appeal rate and a less than one percent overturn rate.
TrueCost is uniquely available as SaaS for payers who choose to manage their payment integrity programs in-house, as full services for those who prefer to outsource the process, or even as a hybrid model where responsibilities are shared between ClaimLogiq and its clients in real-time.
“It can’t be overstated what this technology means: our 15-minute IBill review will enable payers to move to a pre-pay review model – when they previously may not have had the ability to do so. This alone will eliminate millions of dollars in waste by simply not having to pay and chase,” says ClaimLogiq COO, Josh Burrus.
For more information, case studies, and articles detailing ClaimLogiq’s 15-minute IBill review, visit www.claimlogiq.com.
About ClaimLogiq
ClaimLogiq is a healthcare software and technology company that delivers a proactive approach to payment integrity through a powerful, simplified solution. The unique payer-facing, claim-analyzing solution is HITRUST CSF® certified and makes claim reviews accessible to all size healthcare payers for in-depth insight and real-time access into the status of every claim at every stage of the audit lifecycle for controlled, consistent, accurate, and defensible outcomes, second to none. ClaimLogiq’s innovative software stands out from the crowd by allowing payers client-driven control, customizability, and total transparency over the entire claim process and can be applied as a SaaS model, full services, or as a hybrid to suit the specific needs of every payer and provider agreement. ClaimLogiq’s groundbreaking technology produces more cost savings and all-but-removed provider abrasion, impacting millions of lives annually in the pursuit of a higher quality of healthcare for all. For more information, visit www.claimlogiq.com or follow ClaimLogiq on LinkedIn.